Evaluation of the attachment, proliferation, and differentiation of osteoblast
Evaluation of the attachment,proliferation,and differentiation of osteoblast on a calcium carbonate coating on titanium surface
Yi Liu a ,1,Tao Jiang a ,1,Yi Zhou a ,Zhen Zhang a ,Zhejun Wang a ,Hua Tong b ,Xinyu Shen b ,Yining Wang a ,?
a Key Laboratory for Oral Biomedical Engineering,Ministry of Education,School and Hospital of Stomatology,Wuhan University,237Luoyu Road,Wuhan 430079,PR China b
College of Chemistry and Molecular Sciences,Wuhan University,Wuhan 430072,PR China
a b s t r a c t
a r t i c l e i n f o Article history:
Received 9September 2010
Received in revised form 11January 2011Accepted 6March 2011
Available online 11March 2011Keywords:
Calcium carbonate Coating
Surface topography In vitro
Osteointegration
Titanium has been reported to have some limitations in dental and orthopaedic clinical application.This study described a coating process using a simple chemical method to prepare calcium carbonate coatings on smooth titanium (STi)and sandblasted and acid-etched titanium (SATi),and evaluated the biological response of the materials in vitro.The surfaces of STi,SATi,calcium carbonate coated STi (CC-STi)and calcium carbonate coated SATi (CC-SATi)were characterized for surface roughness,contact angles,surface morphology and surface chemistry.The morphology of MG63cells cultured on the surfaces was observed by SEM and Immuno-?uorescence staining.Cell attachment/proliferation was assessed by MTT assay,and cell differentiation was evaluated by alkaline phosphatase (ALP)activity.MG63was found to attach favorably to calcium carbonate crystals with longer cytoplasmic extensions on CC-STi and CC-SATi,resulting in lower cell proliferation but higher ALP activity when compared to STi and SATi respectively.Moreover,CC-SATi is more favorable than CC-STi in terms of biological response.In conclusion,the calcium carbonate coatings on titanium were supposed to improve the osteointegration process and stimulate osteoblast differentiation,especially in early stage.And this method could possibly be a feasible alternative option for future clinical application.
?2011Elsevier B.V.All rights reserved.
1.Introduction
Titanium has been widely used in dental and orthopaedic implants due to its high biocompatibility,excellent mechanical properties and chemical stability [1,2].The biocompatibility of titanium is attributed to its surface oxide ?lm that spontaneously forms when it is exposed to oxygen [3].However,this ?lm with a thickness of 3–10nm is usually very dense and stable,which makes titanium bioinert.The bioinert titanium can only be integrated with bone passively and unable to induce bone apposition [4].In order to improve the bioactivity of titanium and its alloys,various bioactive coatings have been developed,such as calcium phosphate,bioactive glasses and biologically functional molecules.
Currently,plasma spraying is one of the most popular techniques for the preparation of calcium phosphate coatings [5].Short-term clinical and experimental studies have shown that plasma-sprayed hydroxyapatite (HA)-coated implants are able to result in stronger ?xation and faster bone growth rate compared to noncoated implants.However,there are still some concerns about the long term clinical
application of the plasma-sprayed HA-coated implants.Coating delamination and wear debris are reported as major problems associated with these coatings in some long term clinical observations as they cause osteolysis in the surrounding tissue [6,7].
To overcome the drawbacks of plasma-sprayed HA-coated implants,various resorbable coatings,such as biodegradable bone-like carbonate apatite (BCA),octacalcium phosphate (OCP)[8,9],biodegradable Hydroxyapatite [10,11]and resorbable calcium phos-phate [11,12]have been developed.Development of the resorbable coatings is based on the thought that an optimal coating should dissolve in a rate similar to bone formation,and should completely disappear after completion of the bone-healing process [9].The total resorption of the coating may reduce the problems of plasma-sprayed HA-coated implants,which have been mentioned above.
Besides calcium phosphate,calcium carbonate is also an important biomaterial which has been widely used in bone surgery [13,14].There are three crystalline and one amorphous phase of anhydrous calcium carbonates in nature,which are calcite,aragonite,vaterite and amorphous calcium carbonate.It has been demonstrated that calcium carbonate is a biocompatible and osteoconductive material either in the form of aragonite [13,15–17]or in the form of calcite [18].Therefore,calcium carbonate might be an applicable candidate to prepare resorbable coating with improved biodegradation rates due to its higher solubility compared to apatite [19].Recently,Wang et al.[20]successfully fabricated a biologically nacre coating on dental
Materials Science and Engineering C 31(2011)1055–1061
?Corresponding author at:Key Laboratory for Oral Biomedical Engineering,Ministry of Education,School and Hospital of Stomatology,Wuhan University,237Luoyu Road,Wuhan 430079,PR China.Tel.:+862787646696;fax:+862787873260.
E-mail address:wang.yn@https://www.360docs.net/doc/d68225793.html, (Y.Wang).1
Contributed equally to this
work.0928-4931/$–see front matter ?2011Elsevier B.V.All rights reserved.doi:
10.1016/j.msec.2011.03.003
Contents lists available at ScienceDirect
Materials Science and Engineering C
j ou r n a l h o me pa g e :ww w.e l s ev i e r.c o m/l o c a t e /ms e c
titanium implants,where the main component is aragonite.The process of the coating is interesting,but complicated and time-consuming.
The aim of the study was to prepare calcium carbonate coatings on smooth and rough titanium surfaces using a simple chemical treatment,and evaluate the behavior of MG63osteoblast-like cell on these surfaces.Four groups were investigated:smooth titanium (STi),sandblasted and acid-etched titanium(SATi),calcium carbonate coated STi(CC-STi)and calcium carbonate coated SATi(CC-SATi). After analyzing the properties of the surfaces,osteoblastic cell attachment,morphology,proliferation and differentiation were studied.
2.Materials and methods
2.1.Sample preparation
2.1.1.Preparation of STi and SATi
Commercially pure titanium discs,measuring15mm in diameter and1mm in thickness,were used as substrates.STi and SATi discs were prepared according to the following steps:
?STi:titanium discs were wet-ground with120,600,and1500grit silicon carbide abrasive sandpapers,and then were passivated in 50%nitric acid.
?SATi:titanium discs were?rstly prepared in the same way as STi, and then were treated as described in our previous article[21].In brief,the discs were grit-blasted with0.25to0.50mm corundum grit at5bars for1min.Subsequently,the discs were acid-etched in hydrochloric acid/sulfuric acid(1:1)at65°C for30min.
After the above treatments,the discs were ultrasonically cleaned for15min in acetone,ethanol(70%)and deionized water,and?nally dried at room temperature.
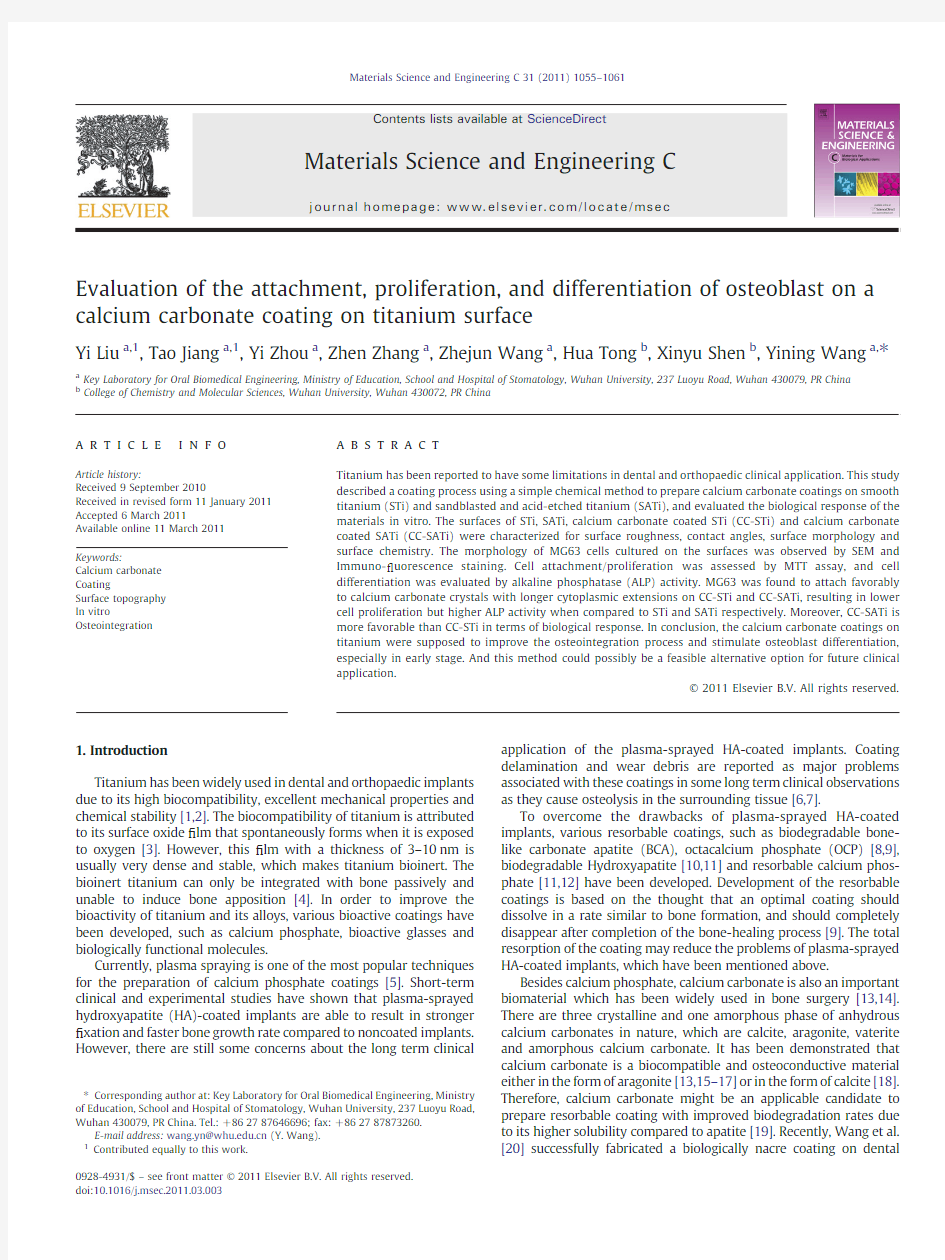
2.1.2.Preparation of CC-STi and CC-SATi
The experimental setup for preparing CaCO3?lms is illustrated in Fig.1.Two vials,one containing a20mM calcium chloride(CaCl2) solution,and the second,containing ammonium carbonate powder, were placed in a desiccator.STi or SATi discs were inverted and placed above the CaCl2solution.CaCO3?lms were then deposited on the STi or SATi substrates via slow diffusion of CO2,produced by decompo-sition of ammonium carbonate at room temperature(4h).The samples were rinsed with deionized water for1min after deposition, and then dried in air overnight.According to this process,CC-STi and CC-SATi discs were produced.
2.2.Surface characterization
Surface roughnesses of the four surfaces were measured using a mechanical pro?lometer(TAYLOR HONSON S4C-3D,England).The contact angles were determined by dynamic contact angle(DCA, Kruss X100,Germany)analysis.Scanning electron microscopy(SEM, Fei QUANTA-200,The Netherlands)was used to investigate the morphology and microstructure of the surfaces.X-ray diffraction (XRD,Bruker AXS D8ADVANCE,Germany)was employed to determine the crystallinity of the materials.The precipitates of CC-STi and CC-SATi were investigated by Fourier transform infrared spectroscopy(FTIR,Nicolet170SX,USA).
2.3.Cell culture
MG63osteoblast-like cells were used for these experiments because they exhibit several fundamental osteoblast characteristics that are typical of a relatively immature osteoblast[22,23].As a result, they are a good model for examining the early stages of osteoblast differentiation.
For all experiments,MG63cells were cultured on disks placed in 24well plates(Corning,Corning,IL).Cells were plated at5000cells cm2in Dulbecco's modi?ed Eagle's medium(DMEM)containing10% fetal bovine serum(FBS),1%penicillin/streptomycin(In-Vitrogen Corporation)and1%L-glutamine(In-Vitrogen Corporation)at37°C in a humidi?ed atmosphere of5%CO2in air.Media were changed every48h until the cells reached con?uence.Because of the opacity of the Ti disks,there was no practical way to assess con?uency of the cultures.As a result,when cells reached visual con?uence on plastic, cultures on all other surfaces were treated exactly as those grown on plastic.
2.4.Immuno-?uorescence staining
After48h of incubation,samples were washed twice with pre-warmed PBS,?xed in4%v/v paraformaldehyde for15min.Each of the samples was then permeabilized in PBS,pH7.4containing0.1%Triton X-100and100mM glycine for30–40min at room temperature, followed by blocking with1%w/v bovine serum albumin(BSA)in PBS at room temperature.Actin?laments were stained with rhodamine phalloidin(1:200in PBS).Nuclei were counterstained with1mg/mL 4,6-Diamidina-2-phenylin(DAPI,Sigma)for10min.Samples were washed with PBS,mounted with Vectashield(Vector)in glass slides and photographed with an inverted?uorescence microscope Axiovert M100(Carl Zeiss).
2.5.Cell morphology
Cell morphology was observed by SEM after2days of culture for the four surfaces.Tested and control cultures were?xed with2% glutaraldehyde in0.1M sodium cacodylate buffer pH7.2(Sigma)for 30min.After washing in the same buffer,dehydration was carried out by sequential immersion in serial diluted solutions of60,70,80,90, and95%v/v ethanol in water,followed by immersion in99.8%v/v ethanol.The samples were then air-dried under laminar?ow at room temperature overnight,coated with gold and examined by SEM.
2.6.Initial cell adhesion and cell proliferation
Cellular adhesion/proliferation was determined by a MTT assay. For the adhesion/proliferation evaluation,cells were cultured on samples for4,24and72h.Then,cells were incubated in a MTT reagent(5mg/ml in PBS)(Sigma Aldrich)at37°C for4h.After removing the culture medium,dimethylsulfoxide(DMSO)was added onto the specimens to release the colored product into the solution. Cell numbers can be assessed by measuring the optical density of the solution at570nm with an El x808Ultra Micro plate Reader(BioTek, USA).The blank reference was taken from wells without cells,also incubated with the MTT solution.Results were expressed as relative MTT activity as compared with control conditions(cells cultured on STi for4
h).
Fig.1.Illustration of the experimental setup.
1056Y.Liu et al./Materials Science and Engineering C31(2011)1055–1061
2.7.Alkaline phosphatase(ALP)activity
For ALP activity evaluation,cells were cultured on samples for3 and6days.At harvest,cell layers were washed twice with phosphate buffered saline solution(PBS,Gibco).A volume of120ml of distilled water plus6ml of1%Triton X-100was added to each well,the cell layers were carefully scraped and stored at?70°C.ALP activity of cell lysates was assayed using a commercially available kit(Enzyline PAL Standardise50,BioMerieux,France).Just before assaying ALP activity, cell lysates were thawed and treated by sonication on ice for5min. The cell homogenate was incubated with p-nitrophenyl phosphate substrate solution(Sigma-Aldrich,St.Louis,MO,USA)at37°C for 15min,and then stopped by addition of NaOH(0.1N).Absorbance was measured at490nm with an El x808Ultra Micro plate Reader (BioTek,USA).The protein determination was performed by the commercially available Micro BCA Protein Assay Reagent kit(Pierce Chemical Co,Rockford IL,USA).The assay was carried out according to the directions of the manufacturer.For each material,the ratio of enzyme activity(expressed in nanomoles of p-nitrophenol/min)to the mass of protein(expressed in micrograms)was determined.Thus, enzymatic activity is expressed in nmol of p-nitrophenol/min/mg of protein.
2.8.Statistical analysis
Statistical analyses were performed with the use of SPSS10.0for WINDOWS.Values of relative MTT activity and ALP activity were expressed as means±standard deviation.Differences were analyzed with a one-way ANOVA test and the Student–Newman–Keuls multiple comparison test.The signi?cance level was set at P b0.05.
3.Results
3.1.Surface characterization
3.1.1.Surface morphology
SEM micrographs of the STi,SATi,CC-STi and CC-SATi surfaces are shown in Fig.2.STi surfaces presented shadow and parallel grooves (Fig.2A).SATi surfaces contained pits and craters(Fig.2B).The pit exhibited0.5–3μm in diameter and appeared to coalesce and form large craters.Crystals with rhombohedral and needle-like morphol-ogy were observed on the CC-STi and CC-SATi surfaces(Fig.2C and D). They formed discontinuous coatings on the substrate.Some crystals contacted partly with each other and some separated from the neighboring crystals.Gaps between the separated crystals were from several microns to20μm.
3.1.2.Surface roughness
The average roughnesses of the different substrates are shown in Table1.STi surfaces presented a smooth surface with the lowest Ra value.SATi surfaces had Ra values of https://www.360docs.net/doc/d68225793.html,-STi and CC-SATi surfaces exhibited different Ra values around1250nm and 2610nm respectively.
3.1.3.Contact angles
The contact angles of the different substrates are shown in Table1. SATi surfaces were found to be signi?cantly more hydrophobic
than Fig.2.SEM micrographs showing the surface topography of the tested titanium discs(A)STi;(B)SATi;(C)CC-STi;and(D)CC-SATi.bar=100μm.
1057 Y.Liu et al./Materials Science and Engineering C31(2011)1055–1061
STi surfaces.Although there were coatings on CC-STi,no signi ?cant differences in their contact angles were observed between CC-STi and STi surfaces.The same results can also be found between CC-SATi and SATi surfaces (P N 0.05).
3.1.
4.XRD
XRD patterns of the four groups are shown in Fig.3,in which Ti denotes peaks from titanium,C denotes peaks from calcite,and A denotes peaks from aragonite.Two crystalline forms of calcium carbonate,Calcite and aragonite,were detected on both CC-STi and CC-SATi surfaces.The intensity of the diffraction peaks of the calcite was strong,while that of aragonite was weak.
3.1.5.FTIR spectroscopy
FTIR spectra of crystals deposited on CC-STi and CC-SATi are presented in Fig.4.It was shown that the precipitates were mainly the mixture of calcite and aragonite.Small amount of vaterite could be detected on CC-STi surfaces.Two sharp absorption bands were found at 876and 713cm ?1,which was the characteristic frequency of well-formed calcite [24].The spectra also displayed the characteristic
absorption peaks of aragonite at 855,713,and 700cm ?1.Vaterite was identi ?ed by a speci ?c carbonate bending at 746cm ?1.3.2.Immuno-?uorescence staining
Immuno-?uorescence micrographs of MG63cells after 48h of culture on the STi,SATi,CC-STi and CC-SATi surfaces are shown in Fig.5.After 48h seeding,the cells appeared to adhere well on the surface of the four surfaces.The cells on STi were spindle-shaped and mostly aligned in one direction (Fig.5A,E).Cells on SATi were
Table 1
Average surface roughness (Ra)and water contact angle (θ)measured for the different surfaces used for culturing MG-63osteoblastic cells.
STi
SATi
CC-STi
CC-SATi
Average roughness,Ra (nm)
110±122190±1751250±1002610±200Water contact angle (°)50.5±2.43107.95±6.0952.7±1.67108.35±
2.63
Fig.3.XRD pattern of (A)STi;(B)SATi;(C)CC-STi;and (D)CC-SATi.Ti denotes peaks from titanium,C denotes peaks from calcite,and A denotes peaks from
aragonite.
Fig.4.FTIR spectra of CaCO 3crystals deposited on STi (A)and SATi (B).
1058Y.Liu et al./Materials Science and Engineering C 31(2011)1055–1061
polygonal in shape and had spread less than those on STi (Fig.5B,F).The morphological appearance of the cells on CC-STi was different from that on STi,which were polygonal in shape (Fig.5C,G).On the CC-SATi surfaces,the cells exhibited more cytoplasmic extension than those on the SATi surfaces (Fig.5D,H).3.3.Cell morphology
SEM micrographs of cells after 48h of culture on the four kinds of surfaces are displayed in Fig.6.The MG63cells spread closely to the STi surfaces with ?lopodia along the periphery of cells,whereas the cells on the SATi surfaces showed a smooth cell membrance with fewer ?lopodia.Cells on the CC-STi and CC-SATi disks had longer cytoplasmic extensions,and attached favorably with calcium carbon-ate crystals.
3.4.Cell attachment and proliferation
Cell attachment/proliferation of MG63cells cultured on the four surfaces is shown in Fig.7.At 4h,the greatest number of cells was found on SATi surfaces.Number of cells on both coated surfaces was fewer than on noncoated ones,while those on CC-STi were less than on CC-SATi (P b 0.01).Between 24and 72h,the number of cells on the four surfaces increased with time and cell proliferation was the highest on the STi surfaces.At 72h,The numbers of cells grown on the surfaces were as follows:STi N SATi N CC-STi N CC-SATi (P b 0.01).3.5.ALP activity
ALP activity of cells cultured on four surfaces is presented in Fig.8.The ALP activity increased with time.No signi ?cant difference in ALP activity was found among the four groups at day 3(P N 0.05).Cells on the CC-SATi surfaces exhibited the highest enzymatic activity at day 6.The ALP activity of cells on the four surfaces was as follows:CC-SATi N SATi N CC-STi N STi (P b 0.01).4.Discussion
In the present study,discontinuous coatings of calcium carbonate were prepared on both smooth and rough titanium using a simple chemical treatment.The discontinuous coating may have several advantages:it combines the merits of both calcium carbonate and the original surface such as sandblasted and etched surface;the coating is easy to be resorbed in vivo;the coating is not easy to be peeled off from the substrates especially on the sandblasted and etched surface.
Calcium carbonate is an important biomaterial which has been widely used in bone surgery [13,14].It has been demonstrated that both calcite and aragonite promote differentiation of human bone marrow cells and have a high level of speci ?c cytocompatiblility [18].Both XRD and FTIR results indicated that the main component of the coating was calcite accompanied by aragonite as minor component.A small amount of vaterite was also detected by FTIR but not by XRD on CC-STi.The reason for this might be the method we have used.The coating was measured in situ by XRD,but was scraped from several disks for FTIR assay.The amount of vaterite in the coating might be too small to be detected by XRD.
Our results of SEM and immune-?uorescence staining indicated that cells on STi and SATi presented different morphology,and calcium carbonate coating had signi ?cant in ?uence on cell spreading on the substrate.After 48h culture,cells on STi showed a cell membrance with many ?lopodia in all direction during attachment and spreading,whereas those on SATi surfaces showed a smooth cell membrance.One possible explanation is that cells supported by ridges and pitches do not need to express a distinctive action network whereas cells on a smooth surface have to spread and develop a strong actin network in order to stabilize themselves on the surface [25].Compared with STi and SATi,cells on the CC-STi and CC-SATi surfaces had longer cytoplasmic extensions,and attached favorably with caicium carbonate crystals.It is well known that surface chemistry and topography of implants in ?uence osteogenic cell responses to the materials [26,27].The calcium carbonate coating changed not only the surface chemistry but also topography of the materials.Calcium carbonate crystals,especially rhombohedral ones,made the surfaces rougher than the original ones.The distance between neighboring crystals is from a few microns up to 20μm,which sizes are close to cells.It has been suggested that pits,protrusions,and steps of dimensions similar to those cells can cause a change of the cell morpholog and alter the activity of biomaterials as compared with ?at surfaces [28].Although calcium carbonate coatings changed the roughnesses of STi and SATi,no signi ?cant differences in their contact angles were observed between CC-STi and STi.The same result can also be found between CC-SATi and SATi.High surface energy,considered as an important variable,is found to be insuf ?cient to cause marked increases in osteoblast responses to Ti substrates with low surface roughness.In contrast,when substrates with complex micron-scale and submicron scale roughness are fabricated to retain the high surface energy of uncontaminated TiO 2,the cells
exhibit
Fig.5.Immuno-?uorescence micrographs showing MG63osteoblastic cell morphology after 2days of culture on (A)STi;(B)SATi;(C)CC-STi;and (D)CC-SATi.bar =100μm.(E)STi;(F)SATi;(G)CC-STi;and (H)CC-SATi.bar =10μm.The nuclcus was stained with DAPI (blue)and the actin network with rhodamine phalloidin (red).
1059
Y.Liu et al./Materials Science and Engineering C 31(2011)1055–1061
synergistic enhancement of their response to the surface topography alone[29].
In this study,the calcium carbonate coatings slightly reduced the initial cell attachment despite it favored the cell spreading.Several studies have demonstrated that rough titanium surfaces increase the cell attachment as compared to smooth ones[30–32].In the present study,SATi also showed higher cell attachment at4h culture than STi, which is consistent with previous studies.However,CC-STi and CC-SATi exhibited less cell attachment than STi and SATi respectively despite of their higher surface roughness.This effect should be related to the surface chemistry of the coating.It has been reported
that
Fig.7.Cell attachment/proliferation of MG63cells cultured on the titanium surfaces for4,
24and72h.The MTT activity was measured as optical density in triplicate and two series
of experiments(n=6),and normalized to cells cultured on STi for4h(100%)in order to
demonstrate differences in cell viability on the titanium substrates.*P b0.05,**P b
0.01.
Fig.8.ALP activity of MG63cells cultured on STi,SATi,CC-STi and CC-SATi at3and6days.
Values represent the mean±SD of triplicate measurements.*P b0.05,**P b
0.01.
Fig.6.SEM micrographs of MG63osteoblastic cell morphology after2days culture on(A)STi;(B)SATi;(C)CC-STi;and(D)CC-SATi.bar=10μm.The white arrows indicate the cells. The black arrows indicate the calcium carbonate crystals.
1060Y.Liu et al./Materials Science and Engineering C31(2011)1055–1061
titanium surface with high level of calcium ion implantation could inhibit cell attachment[33].
ALP activity is a marker of bone cell differentiation and is commonly used as an indicator for osteogenesis[34].The present study showed that the cell proliferation decreased at24H and72H while ALP activity increased at day6in SATi as compared with STi. This indicated that the sandblasted and etched surface in?uenced the cell proliferation at early time,while the cell differentiation at later time.The results were consistent with the previous studies,which suggested that differentiation toward an osteoblastic phenotype correlates with a decrease in cell proliferation and an increase in ALP activity[26,35].Meanwhile,the cell proliferation and ALP activity displayed the same trend when CC-STi and CC-SATi were compared with STi and SATi respectively,which indicated that calcium carbonate coating might induce cell differentiation toward an osteoblastic phenotype.This effect is probably related to the surface roughness and calcium ion release from the calcium carbonate coating.It has been proved that rough surfaces favor the differenti-ation of MG63cells and higher Ca2+concentrations also promote osteoblast differentiation,leading to bone mineralization[36].
It was interesting to note that CC-SATi promoted more favorable biological responses than CC-STi and SATi in the study.This should probably be attributed to the synergistic effect of discontinuous calcium carbonate coating and the original sandblasted and etched surface.It has been well documented that combination of sandblast and acid etching could produce macro-roughness and micro-rough-ness on titanium surface,which achieves better biological responses in vitro and vivo as compared to smooth surface[21,32].Our results suggested that the biological performance of the surface was further improved when calcium carbonate coating was prepared on the sandblasted and etched surface.Thus,it is reasonable to expect that CC-SATi may have better performance in the in vivo situation.
It should be pointed out that the bond strength of the coating could not be appropriately evaluated using conventional methods such as shear,tensile or scratch test because the coating was discontinuous. However,it was found that the coating was hard to be scraped from CC-SATi surfaces during the FTIR test.Moreover,our ongoing in vivo experiment indicated that CC-SATi could withstand peeling of coatings during implant procedure.
5.Conclusions
The results in the present study suggest that calcium carbonate coating may favor a better biological outcome of titanium implants in vivo,since it may induce differentiation toward an osteoblastic phenotype,and therefore enhance the osteointegration process especially in early stage.Of the two kinds of calcium carbonate coated surfaces,CC-SATi is more favorable.Further in vivo studies with animal models are necessary for a better understanding of the osteointegration properties of calcium carbonate coated titanium.Acknowledgements
This work was supported by grant No.30872910from the National Natural Science Foundation of China,No.2007BAI18B05from the National Key Technology R&D Program of China during the11th Five-year Plan and Science and Technique Foundation from Bureau of Health of HuBei Province,China.
References
[1]P.M.Brett,J.Harle,V.Salih,R.Mihoc,I.Olsen,F.H.Jones,M.Tonetti,Bone35
(2004)124.
[2]J.B.Nebe,L.Muller,F.Luthen,A.Ewald,C.Bergemann,E.Conforto,F.A.Muller,
Acta Biomater.4(2008)1985.
[3]J.Black,Clin.Mater.16(1994)167.
[4]J.W.Park,J.Y.Suh,H.J.Chung,J.Biomed.Mater.Res.A86(2008)117.
[5]J.Forsgren,F.Svahn,T.Jarmar,H.Engqvist,Acta Biomater.3(2007)980.
[6]T.Albrektsson,J.Oral Maxillofac.Surg.56(1998)1312.
[7]M.Rokkum,A.Reigstad,C.B.Johansson,Acta Orthop.Scand.73(2002)298.
[8]T.Kikawa,O.Kashimoto,H.Imaizumi,S.Kokubun,O.Suzuki,Acta Biomater.5
(2009)1756.
[9] F.Barrere,C.M.van der Valk,R.A.Dalmeijer,C.A.van Blitterswijk,K.de Groot,P.
Layrolle,J.Biomed.Mater.Res.A64(2003)378.
[10] E.C.S.Rigo,A.O.Boschi,M.Yoshimoto,J.S.Allegrini,J.B.Konig,M.J.Carbonari,
Mater.Sci.Eng.C24(2004)647.
[11]P.Peng,S.Kumar,N.H.Voelcker,E.Szili,R.S.Smart,H.J.Griesser,J.Biomed.Mater.
Res.A76(2006)347.
[12] A.Bernstein,D.Nobel,H.O.Mayr,G.Berger,R.Gildenhaar,J.Brandt,J.Biomed,
Mater.Res.B Appl.Biomater.84(2008)452.
[13] A.Piattelli,G.Podda,A.Scarano,Biomaterials18(1997)623.
[14]R.A.Yukna,C.N.Yukna,J.Clin.Periodont.25(1998)1036.
[15]T.Turunen,J.Peltola,H.Helenius,A.Yli-Urpo,R.P.Happonen,Clin.Oral Implant.
Res.8(1997)96.
[16]U.Ripamonti,J.Crooks,L.Khoali,L.Roden,Biomaterials30(2009)1428.
[17]L.Abramovitch-Gottlib,S.Geresh,R.Vago,Tissue Eng.12(2006)729.
[18]J.C.Fricain,R.Bareille,F.Ulysse,B.Dupuy,J.Amedee,J.Biomed.Mater.Res.42
(1998)96.
[19] F.Braye,J.L.Irigaray, E.Jallot,H.Oudadesse,G.Weber,N.Deschamps, C.
Deschamps,P.Frayssinet,P.Tourenne,H.Tixier,S.Terver,J.Lefaivre,A.Amirabadi, Biomaterials17(1996)1345.
[20]X.X.Wang,L.Xie,R.Wang,Biomaterials26(2005)6229.
[21]Y.Zhou,T.Jiang,M.Qian,X.Zhang,J.Wang,B.Shi,H.Xia,X.Cheng,Y.Wang,
Biomaterials29(2008)461.
[22]J.Clover,M.Gowen,Bone15(1994)585.
[23]R.T.Franceschi,W.M.James,G.Zerlauth,J.Cell.Physiol.123(1985)401.
[24]M.B.Saffo,H.A.Lowenstam,Science200(1978)1166.
[25]T.P.Kunzler,T.Drobek,M.Schuler,N.D.Spencer,Biomaterials28(2007)2175.
[26]J.Lincks,B.D.Boyan,C.R.Blanchard,C.H.Lohmann,Y.Liu,D.L.Cochran,D.D.Dean,
Z.Schwartz,Biomaterials19(1998)2219.
[27] C.Wirth,B.Grosgogeat,https://www.360docs.net/doc/d68225793.html,gneau,N.Jaffrezic-Renault,L.Ponsonnet,Mater.Sci.
Eng.C28(2008)990.
[28] B.Kasemo,J.Gold,Adv.Dent.Res.13(1999)8.
[29]G.Zhao,A.L.Raines,M.Wieland,Z.Schwartz,B.D.Boyan,Biomaterials28(2007)
2821.
[30]H.H.Huang,C.T.Ho,T.H.Lee,T.L.Lee,K.K.Liao,F.L.Chen,Biomol.Eng.21(2004)93.
[31]K.Anselme,M.Bigerelle,Acta Biomater.1(2005)211.
[32] D.D.Deligianni,N.Katsala,https://www.360docs.net/doc/d68225793.html,das,D.Sotiropoulou,J.Amedee,Y.F.Missirlis,
Biomaterials22(2001)1241.
[33]S.N.Nayab,F.H.Jones,I.Olsen,Biomaterials26(2005)4717.
[34]M.Bachle,R.J.Kohal,Clin.Oral Implant.Res.15(2004)683.
[35] B.D.Boyan,R.Batzer,K.Kieswetter,Y.Liu,D.L.Cochran,S.Szmuckler-Moncler,
D.D.Dean,Z.Schwartz,J.Biomed.Mater.Res.39(1998)77.
[36]S.Maeno,Y.Niki,H.Matsumoto,H.Morioka,T.Yatabe,A.Funayama,Y.Toyama,T.
Taguchi,J.Tanaka,Biomaterials26(2005)4847.
1061
Y.Liu et al./Materials Science and Engineering C31(2011)1055–1061
