药物毒性试验的设计
Optimising the design of preliminary toxicity studies
for pharmaceutical safety testing in the dog
David Smith a, , , Robert Combes b , Olympe Depelchin c , Soren Dyring Jacobsen d , Ruediger Hack e , Joerg Luft f , Lieve
Lammens g , Friedrich von Landenberg h , Barry Phillips i , Rudolf Pfister j , Yvon Rabemampianina k , Susan Sparrow l , Claudia Stark m and Markus Stephan-Gueldner n
a AstraZeneca, Alderley Park, UK
b FRAME, Nottingham, UK
c Lilly, Mont-Saint Guibert, Belguim
d NovoNordisk, Maaloev, Denmark
e Aventis, Frankfurt, Germany
f AltanaPharma, Hamburg, Germany
g Janssen, Beerse, Belgium
h Merck KGaA, Darmstadt, Germany
i RSPCA, Horsham, UK
j Novartis Pharma, Basel, Switzerland
k Pfizer, Amboise, France
l GlaxoSmithKline, Ware, UK
m Schering AG, Berlin, Germany
n Hoffmann-La Roche AG, Basel, Switzerland
Abstract
A working party, comprising two animal welfare organisations and
some 12 pharmaceutical companies in Europe, was established to minimise the use of the dog in safety testing. As first step, the
participants defined the major objectives of preliminary dose-range finding/MTD toxicity studies in non-rodents, defined the principles and requirements for this study type and agreed on a proposal for an optimised study design, based on collective experience of conducting such studies in industry, involving an evaluation of 100 individual study data sets. The suggested study design is explained and
described, and reflects current best practice in the pharmaceutical industry in Europe. The implementation of such an optimised design is believed to result in a reduction in the overall numbers of animals used for this purpose, without jeopardising the scientific rationale and b b s .y a o z h .c o m
usefulness of the studies for informing the conduct of later regulatory studies.
Keywords: Reduction; Refinement; Alternatives; Animal use; Dogs; Laboratory animal science; Toxicity tests; Regulatory toxicology
1. Introduction
1.1. Background
The pharmaceutical industry recognises the need to implement
strategies for reducing, refining, and replacing the use of animals in toxicity studies (The Three Rs) (Tweats, 2000), particularly regarding the use of companion species in safety testing (Baker and Broadhead, 2000). To this end, several pharmaceutical companies based in Europe have formed a working party with two scientific and animal welfare charities in the UK, the Royal Society for the Prevention of Cruelty to Animals (RSPCA) and the Fund for the Replacement of Animals in Medical Experiments (FRAME). The formation of this collaborative group in 2000 was prompted by a recommendation made at a workshop held to discuss the use of the dog as a second species in regulatory toxicity testing, which in turn was organised as a result of some preliminary research conducted by FRAME and the RSPCA (Broadhead et al., 1998, Broadhead et al., 1999 and Broadhead et al., 2000).
The principal remit of the working party is to propose and, where possible, put into practice scientifically valid and feasible approaches to optimise dog use in the safety evaluation of pharmaceuticals, without compromising human safety or increasing the use of other non-rodent species. 1.2. Initial approach—analysis of the design of
preliminary repeat dose toxicity studies
As one of its first tasks, the working party identified many potential approaches for optimising dog use, and these have been prioritised for further consideration (Smith et al., 2002). One promising
approach related to the design of repeat dose toxicity studies, and included a comprehensive analysis of the different designs currently b b
s .y a o z h .c o m
being used by the member companies of the working party for preliminary escalating dose/maximum tolerated dose (MTD) and dose range finding (DRF) studies, which precede pivotal repeat dose toxicity testing. The objective of this investigation was to define the principles and requirements of MTD and DRF studies so that an optimised study design could be identified. Such a design should deliver appropriate early information on the characteristics of the test compound in non-rodents and allow a reliable prediction of appropriate dose levels for the 14 day/1 month regulatory toxicity study, thus achieving the most effective use of the animals. The information from this optimised study design should also meet single dose (acute) toxicity study requirements.
1.3. Objective of the paper
We intend to share the results of our co-operation and propose an optimised study design, which was formulated as a result of the sharing of data, current working practices, and experiences among members of the working party. Publication of this paper is also intended to promote dialogue with other toxicologists in the industry, and with regulators, who are involved with generating data based on these tests, or who have to assess such information. The work described in this manuscript is part of a wider effort by the working party to optimise and minimise the use of the dog as a second species in the regulatory safety assessment of new pharmaceuticals. Preliminary findings have been published elsewhere (Phillips et al., 2004; Smith et al., 2003). 2. Results of discussions 2.1. The purpose of preliminary studies
The sharing of information between members of the collaborative group soon revealed that, although each organisation used the MTD/DRF study to select dose levels for the repeat dose, regulatory study, the additional uses to which this study were put varied greatly between companies. As a consequence of this difference in custom and practice between each company, different study designs were in use in nearly all cases. b b s .y a o z h .c o m
In consequence, agreement was sought on the primary and
secondary purposes of such studies, together with reaching
consensus on the nature of any optional data sets that could also be generated, before an optimised protocol could be developed. The results of this discussion exercise are summarised in Table 1 and Table 2.
Table 1. Primary and secondary purposes of preliminary DRF/MTD study in the dog Purpose Description
Primary Dose selection (highest dose) for the pivotal repeat dose studies conducted prior to first dose to man
Secondar
y Detection of serious toxicity (often referred to as target organ toxicity) to confirm the selection of candidate drugs
Obtaining toxicokinetic data at a range of doses to allow optimal dose selection for subsequent repeat dose studies in relation to estimated clinical doses
Assessment of suitability of the dog as the second species
Also used for estimating compound requirements for the subsequent repeat dose studies able 2.
Further information obtainable from preliminary MTD/DRF studies in the dog Parameter
Comments No observed effect level (NOEL)
After single or multiple doses
No observed adverse effect level (NOAEL)After single or multiple doses
Systemic exposure
Measured at each dose level in plasma
Overt clinical signs Characterisation of overt toxicity after single or multiple doses b b s .y a o z h .c o m
Parameter Comments
Dose proportionality Saturation of absorption/elimination
Tachyphylaxis Induction after multiple doses
Tolerability/responsiveness To confirm species selection
Delayed onset of toxicity During the repeat dose phase
Recovery from toxic insult After single or multiple doses, e.g., clinical signs
Clinical pathology Within the constraints of the design After considerable discussion concerning the intended uses of maximum tolerated dose (MTD) and dose range finding (DRF) studies, it was agreed that an MTD study should be designed to detect a tolerance limit based on the results of an in vivo test, following the administration of single, escalating doses of test chemical. It was also agreed that DRF studies should be designed to identify a tolerance limit following the repeated administration of the highest feasible dose, based on the outcome of an MTD study. The working party paid particular attention to make suggestions for improving the design of the MTF/DRF preliminary studies that would allow the collection of data compatible with further regulatory
requirements for non-rodent safety testing, so as to avoid
compromising its overall objective of minimising dog usage. To this end, proposals for a new study design were made so that data
generated by the new protocol would meet the requirements to
replace the single dose (acute) toxicity study in non-rodents, since according to the experience of some members of the working party, the strategy of using MTF/DRF data instead of especially generated single dose toxicity data in non-rodents is well accepted by some regulators (namely those in Japan), which still request this type of information collected in non-rodents. Moreover, some regulatory guidelines provide sufficient flexibility to cater for the submission of b b s .y a o z h .c o m
data obtained in this manner (FDA Guidance for Industry, 1996:
Single Dose Acute Toxicity Testing for Pharmaceuticals; Yakuji Nippo, Japan’s and ICH guidelines for new drug registration, 1999). In addition to the primary and secondary purposes of MTD/DRF studies, the working group identified further information that could also be obtained or derived from such studies (Table 2).
The usefulness of including each of the above requirements in any study design is discussed later. It is most important to balance the welfare implications of intensive animal handling, treatment
procedures and sampling methods with the overall number of dogs used when designing studies.
2.2. Factors affecting design The following factors were considered by the working party to influence the design of any MTD/DRF study. It should, however, be noted that the following list is unlikely to be exhaustive, but reflects the current approach to drug development. 2.2.1. The overall number of animals required The total number of animals per study depends on the number of dose groups and the group size. Thus, any approach to minimise the total number of animals used has to target on limiting the number of separate dose groups and on minimising the group size needed to achieve a sufficient and relevant data set. If it is accepted that such studies are only designed to detect
significant levels of toxicity, then it is possible to use small group sizes, without control animal groups. Data presented later show that the relevance and predictability of such studies do not correlate to the group sizes used, although the fact that there are limits to reducing group sizes should be recognised. 2.2.2. The amount of compound available for
testing It is, of course, mandatory for such studies to have sufficient chemical, or drug supply to allow inclusion of dose levels high enough to b b
s .y a o z h .c o m
produce significant toxicity. Restriction of dose-escalation due to limitation of compound supply can seriously compromise the validity of the preliminary study, for example, due to a failure to identify target organ toxicity, and in consequence can jeopardise the outcome of a subsequent regulatory 14 day/1 month study. Study designs that entail the use of minimal numbers of animals result in parallel in a minimisation of compound need per dose step and thus allow testing of high doses up to the maximum recommended dose (2 g/kg) and a prolongation of repeat dose treatment.
2.2.
3. The use of previous information
Despite the fact that company practices vary, it is not unusual to have information from in vitro and in vivo low dose pharmacokinetic studies, prior to conducting a MTD/DRF study. However, such data are rarely generated in dogs. In addition, safety pharmacology studies in
telemetered dogs may have been performed. Data from these studies, together with those from rodent studies (in general performed before dog studies), should be used to design the MTD/DRF dog study.
2.2.4. Pharmacological class
The mode of action of a test compound can influence the design of the study, for example cell cycle inhibitors that preclude the re-dosing of animals, due to delayed onset of toxicity.
2.2.5. Compound attributes
The physico-chemical properties of a compound, together with its ADME profile (absorption, distribution, metabolism, and excretion), and its intended route of administration, might be such as to require a non-standard study design to be considered. Compounds with very short or very long elimination half-lives fall into this category. 2.2.6. The timing of a study
The total duration of a study may impact the progression of a
compound during the drug development process. In the very early pre-nomination (research) phase of compound development,
information about toxicity or pharmacological activity might be an essential go/no go criterion for further development. When the test is b b
s .y a o z h .c o m
conducted close to first use in man, the availability of the results of the study might be time-limiting for the commencement of the pivotal 14 day/1 month study. In both scenarios, however, there is pressure to minimise study duration.
2.2.7. The need to replace the acute toxicity study
There was general consensus that standard acute toxicity studies in dogs should be omitted. Some members confirmed that data from escalating, or short-term, repeat dose studies had been accepted as acute toxicity data in non-rodents by Japanese regulatory bodies. The regulatory guidelines for both USA and Japan, which still recommend acute toxicity testing in non-rodents, offer this flexibility (FDA
Guidance for Industry, 1996: Single Dose Acute Toxicity Testing for Pharmaceuticals and Yakuji Nippo Ltd, Japan’s and ICH guidelines for new drug registration, 1999). The essential information required by such regulators for such studies in the non-rodent appear to be: (a) identification of dose levels provoking overt signs of toxicity; (b)
inclusion of appropriate parameters and sufficiently long observation periods proper observations (no more details given); and (c)
conducted according to GLP regulations (see below).
No recommendations are made in the guidelines, however, on the number of animals that should be used, but custom and practice indicates that 2 male and 2 female animals are acceptable.
2.2.8. Conducting studies according to GLP regulations
There is a requirement to conduct the dog MTD/DRF study according to GLP standards if information from this study is to be used for risk assessment in man. When this study is performed early in the developmental programme, however, it is neither possible nor necessary to fulfil all the requirements of GLP. Regulators have accepted such studies provided that: (a) the study has been
performed in a GLP compliant facility; (b) the study plan, conduct, and report are subject to audit; (c) an impurity profile is generated in lieu of a compound specification; (d) non-validated methods for
analysis of drug substance and toxicokinetics are documented in lieu b b s .y a o z h .c o m
of fully validated methods; and (e) all deviations from GLP compliance are noted.
2.2.9. The duration of dosing
The predictiveness of the study is increased with increasing duration of the repeat dose phase. However, as with many of the other factors, the ability to increase the duration of dosing has to be balanced
against compound availability and efficiency (speed). It was apparent that most of the companies in the working group have adopted 5–7 days as the default duration, although 14 days is used by some.
3. Obtaining information on current practice The Steering Group distributed questionnaires to companies that were aimed to: (a) elicit current designs of both MTD and DRF phases of the study and (b) examine the outcome of the most recent studies (at least 10) conducted by each organisation.
3.1. Current designs for the MTD/DRF study
The main reasons for the discrepancies in the various designs for the study by individual companies are: (a) the different emphasis that each company applies to the purpose of the study; (b) variations in the extent of data sets each company wishes to generate; and (c) the confidence that each company requires before conducting the subsequent pivotal 14 day/1 month study.
However, it was apparent that most companies use a two-phase
design involving the administration of an escalating dose, followed by repeat dosing, although some important general and many detailed differences became obvious when the designs were compared (Table 3 and Table 4).
Table 3. Examples of high level design differences in the MTD/DRF study An escalating phase followed by repeat dosing
An escalating phase only
Repeat dosing only
An escalating phase during candidate drug selection, with repeat dosing prior to the pivotal study b b s .y a o z h .c o m
An escalating phase followed by repeat dosing
Repeat dosing of 5–14 days duration Table 4. Examples of detailed design differences in the MTD/DRF study
The re-use of animals between different dosing regimens
The re-use of low-dose animals between studies
The use of parallel groups of dogs during escalation phase (resulting in an overall increase in animals)Repeat dosing during the escalation phase
An escalating phase, with or without a washout period
Some of the above differences are clearly due to natural variation in the way laboratories will design experiments to achieve the same aims. However, further differences in the design are also due to the fact that different custom and practice has been established such that the study can variously be used to establish NOAEL values, provide off-dose recovery data, and meet the needs of the single dose (acute) study. The existence of such diversity in designs for the study is, therefore, not surprising. 3.2. Sharing data to develop a common study design Compound data sets were generated by each participating company from previous studies to reveal: (a) the number of dogs used in the escalating phase of the study; (b) the number of dogs used in the repeat dose phase; (c) the therapeutic indication area of a given project; (d) what route of administration had been used; and (e) the outcome of the subsequent pivotal 14 day/1 month study in terms of whether it was judged a success or a failure.
It was agreed that the criterion for judging whether the MTD/DRF study had been successful was the ability to select an appropriate high dose level for the subsequent pivotal 14 day/1 month study that elicited target organ toxicity or, defined the maximum technically feasible dose. The MTD/DRF study was judged a failure if additional animals or an additional dose group had to be used in the 14 day/1 month study, or if this study had to be repeated due to inappropriate dose selection.
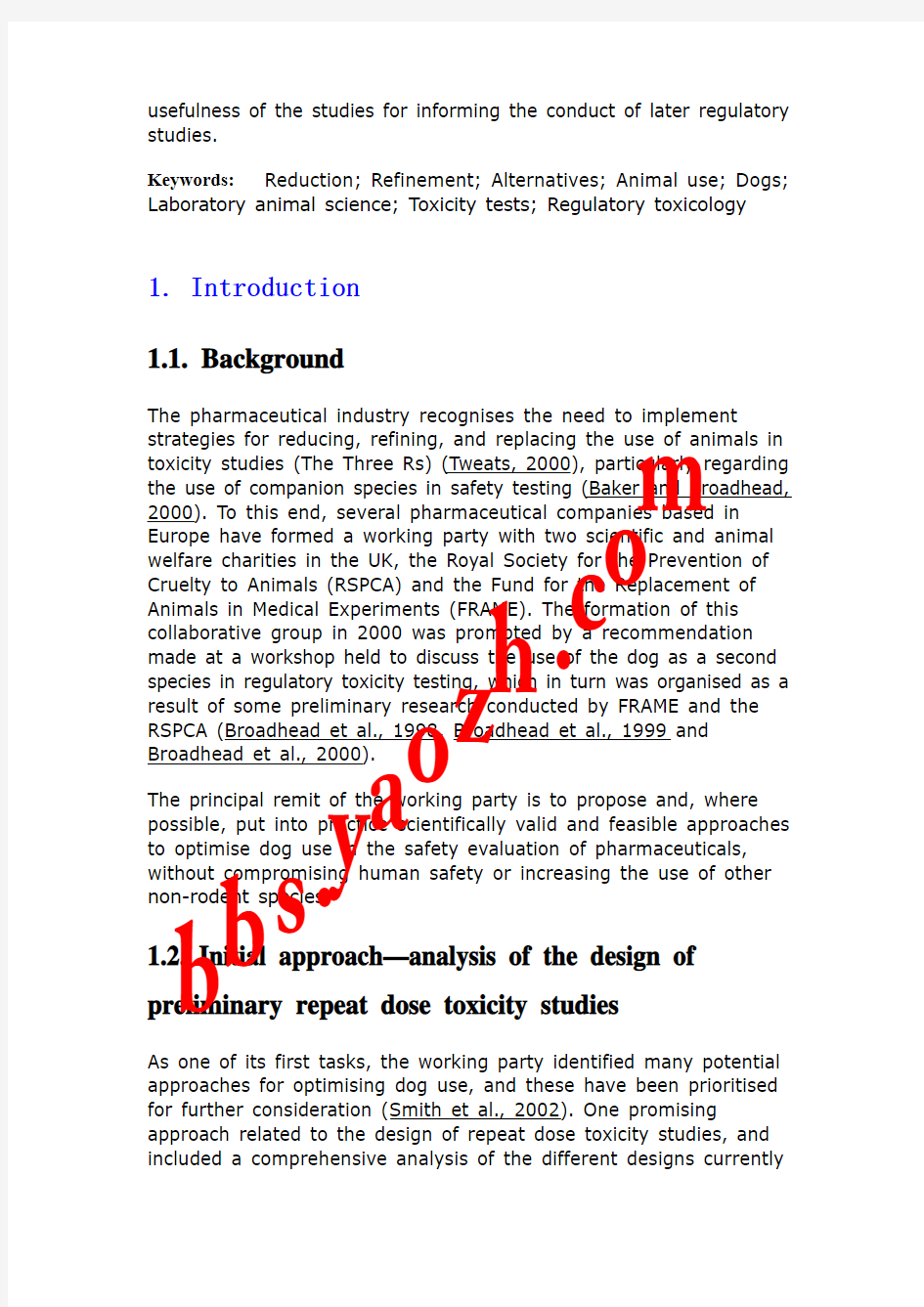
An analysis of the results from 101 pivotal 14 day/1 month studies is illustrated in Fig. 1. The data show that preliminary dose-setting studies that involved the use of up to 4 dogs are as likely to be b b s .y a o z h .c o m
successful in predicting appropriate dose levels for the subsequent 14 day/1 month study, as are those studies that involved substantially more.
Fig. 1. Number of animals vs. success or failure.
For those tests classified as having failed, the cause could not be attributed to drug target or therapy area (Table 5).
Table 5. Study outcome related to therapy area Therapy area Number of compounds
Success
Failure Metabolism 12
2 CNS
28 4
Cardiovascular 16 3 Inflammatory 2 — Oncology 8 — GI tract
6 — Respiratory
8 1 Infection
6 — Dermal
1 — Urogenital
1 — Hormonal
2 — Imaging 1 — It is not possible to assess whether route of exposure affected the outcome of the studies as the oral route was used in 95/101 cases with intravenous, intravenous infusion, and subcutaneous injection each used in 2 studies. All of these six studies were classified as b b
s .y a o z h .c o m
success, but the imbalance in the routes of exposure precludes any conclusions being made.
4. Discussion
4.1. A proposal for an optimised study design
Having taken into account the primary objective of the preliminary MTD/DRF studies, and after considering the information generated from the review of previous studies, the Steering Group proposed a basic design involving an escalating dose phase involving one male and one female dog dosed to the MTD, followed by repeat dosing (of >4 days duration) in one male and one female na?ve animal at the MTD, with additionally one male and one female non-na?ve animal at the same dose or a lower dose.
On occasions when animals from the escalating dose phase cannot be re-used in the repeat dose phase (if the MTD is exceeded), a further two animals would be required (total six animals).
The above design has been demonstrated to be satisfactory and should be sufficient for almost all circumstances, although, as is the case with the design of all toxicity studies, it is necessary to consider each project on a case-by-case basis. An alternative design, which has also been shown to be satisfactory and could be considered is a repeat dose study involving three dose levels in one male and one female dog.
Using these basic high-level designs, the toxicologist can then
consider the detailed study parameters, which should be included in a study on a case-by-case basis. These parameters are discussed later. One important factor to consider in the escalating dose phase is the need for adequate wash-out (off dose) between administrations during the dose escalation phase of the study. In the absence of pharmacokinetic data, it is usual to fix the interval between
successive dosings at 2 or 3 days. Care is also needed when
evaluating cytotoxic compounds and those that accumulate in the body or that exhibit delayed toxicity. 4.2. Study parameters b b
s .y a o z h .c o m
Several parameters could be included on a case-by-case basis in an MTD/DRF study and these are listed and briefly discussed in Table 6. Table 6. Parameters that could be included in preliminary MTD/DRF studies in dogs End-point Note
Clinical signs Probably one of the most important parameters both in terms of identifying overt
adverse effects and also managing their outcome. Frequent observation is essential as
this parameter is most likely to be the one to establish the MTD
Body weight A very sensitive indicator of toxicity and regular recordings are important
Food
consumption Closely associated with body weight changes
Water
consumption Rarely measured
Haematology/
clinical
chemistry Should be performed at each dose escalation and at the completion of repeat dose phase. After pathology, it is the laboratory investigation most likely to detect toxicity
Urinalysis
Less useful and could be excluded. May be considered in the future for metabonomics
ECG The value of ECG data on less than 4 dogs is limited and is better obtained from Safety Pharmacology using telemetry. However, because of the higher dose levels used in the MTD study it may be useful to analyse data from the highest dose animals. Measurements should include T max
Blood
pressure
Similar consideration as ECG. Effects on BP will not usually prevent a compound going into man and therefore this parameter is not routine
Toxicokinetics Essential component of each phase. Rapid feedback of plasma level data can avoid
unnecessary dosing of animals when saturation of absorption is observed b b s .y a o z h .c o m
End-point Note
Ophthalmolog
y Investigations are non-invasive and should be considered at the end of the repeat dose phase
Gross
pathology Can indicate additional tissues for pathological examination. Necropsy should be performed within two to three days of cessation of dosing (repeat dose phase)
Histopatholog
y Essential to identify target organ toxicity. Major organs/tissues, abnormal tissues and others on a project-specific basis should be examined
Cytochrome
P450 levels Should be considered if findings from previous rat studies indicate induction of metabolism
5. Conclusions
The work of the Steering Group illustrates an initiative by industry and animal welfare to share unpublished data, with the aim of reducing animal usage, thereby improving animal welfare, without compromising scientific validity. In addition to the intrinsic value of reducing animal numbers the project has also been able to provide a mechanism for adding value to the design of animal studies. The worth of sharing unpublished data has been demonstrated by the ability of the group to propose an optimised design for the preliminary toxicity studies in the dog. These preliminary studies are not
undertaken for regulatory purposes, and so it is possible to make progress without change to the regulatory framework. The proposed designs, involving the use of 4 or 6 dogs, will result in the use of less animals. The actual level of reduction in animal numbers is difficult to quantify, but the overall projected impact is considered to be
significant, bearing in mind the welfare cost to each animal in this type of experiment and the number of such experiments undertaken globally in the pharmaceutical industry. It should also be remembered that these studies are performed early within a project life, and many of the compounds subjected to this study do not progress to the market. b b s .y a o z h .c o m
The recommended study design is supported by the data, but it is nevertheless a compromise based on experience. As with all study designs there might be a need for a ‘case-by-case’ approach for
candidate compounds intended for specific therapeutic areas and for individual requirements for each company.
As a result of our collaborative study, it is recommended that
companies review their study designs with the aim of adopting our proposed new study design for reduced animal numbers. A number of Steering Group members have already done so but not without a change of mind set.
References Baker and Broadhead, 2000 R. Baker and C. Broadhead, Should cats and dogs be used as laboratory animals In: M. Balls, A.-M. vanZeller and M. Halder, Editors, Developments in Animal and Veterinary Sciences, 31B: Progress in the Reduction, Refinement and Replacement of Animal Experimentation , Elsevier, Oxford (2000), pp. 1725–1730. Broadhead et al., 1998 Broadhead, C.L., Jennings, M., Heywood, R., Combes, R.D., 1998. The use of dogs in regulatory toxicology. In: O’Donoghue, P.N. (Ed.), The Ethics of Animal Experimentation: Proceedings of the European Congress held 17–18 December, 1996, at the Palais des Congres, Brussels. EBRA, London, p. 261. Broadhead et al., 1999 Broadhead, C.L., Jennings, M., Combes, R.D., 1999. A Critical Evaluation of the Use of Dogs in the Regulatory Toxicity Testing of Pharmaceuticals. FRAME, Nottingham, UK (ISBN 0 9501 700 5 4), 106 pp. Broadhead et al., 2000 Broadhead, C.L., Betton, G., Combes, R., Damment, S., Everett, D., Garner, C., Godsafe, Z., Healing, G., Heywood, R., Jennings, M., Lumley,
C., Oliver, G., Smith,
D., Straughan, D., Topham, J., Wallis, R., Wilson, S., Buckley, P. (observer) 2000. Prospects for reducing and refining the use of dogs in regulatory toxicity testing of pharmaceuticals. Human and Experimental Toxicology 19, 440–447. Phillips et al., 2004 B. Phillips, D. Smith, R. Combes, G. Descotes, S. Dyring Jacobsen, R. Hack, J. Kemkowski, K. Krauser, R. Pfister, Y. Rabemampianina, S. Sparrow, M. Stephan-Gueldner and F. von Landenberg, An approach to minimise dog use in regulatory toxicology: production of a best practice guide to study design, Alternatives to Laboratory Animals 32S1 (2004), pp. 447–451. Abstract-EMBASE | $Order Document b b s .y a o z h .c o m
Smith et al., 2002 D. Smith, C. Broadhead, G. Descsotes, R. Fosse, R. Hack, K. Krauser, R. Pfister, B. Phillips, Y. Rabemampianina, J. Sanders, S. Sparrow, M. Stephan-Gueldner and S.D. Jacobsen, Preclinical safety evaluation using nonrodent species: an industry/welfare project to minimize dog use, ILAR Journal, Suppl. (2002), pp. 539–542. Smith et al., 2003 D. Smith, R. Combes, G. Descotes, S. Dyring Jacobsen, R. Hack, J. Kemkowski, K. Krauser, L. Lammens, R. Pfister, B. Phillips, Y. Rabemampianina, S. Sparrow, M. Stephan-Gueldner and F. von Landenberg, Approaches to the minimisation of dog use in the safety assessment of pharmaceuticals: an industry/animal welfare initiative, Toxicology Letters 144 (2003) (Suppl. 1), p. 48. Abstract-Compendex | Abstract-INSPEC | $Order Document Tweats, 2000 D. Tweats, A review of the reduction and refinement of regulatory toxicity studies for pharmaceuticals In: M. Balls, A.-M. van Zeller and M. Halder, Editors, Developments in Animal and Veterinary Sciences, 31B: Progress in the Reduction, Refinement and Replacement of Animal Experimentation , Elsevier, Oxford (2000), pp. 783–791.
b b s .y a o z h .
c o m
药物重复给药毒性试验技术指导原则
药物重复给药毒性试验技术指导原则 一、概述 重复给药毒性试验是描述动物重复接受受试物后的毒性特征,它是非临床安全性评价的重要内容。重复给药毒性试验可以:①预测受试物可能引起的临床不良反应,包括不良反应的性质、程度、量效和时效关系、以及可逆性等;②判断受试物重复给药的毒性靶器官或靶组织;③如果可能,确定未观察到临床不良反应的剂量水平(No Observed Adverse Effect Level,NOAEL);④推测第一次临床试验(First in Human, FIH)的起始剂量,为后续临床试验提供安全剂量范围;⑤为临床不良反应监测及防治提供参考。 本指导原则适用于中药、天然药物和化学药物。 二、基本原则 药物安全性评价试验必须执行《药物非临床研究质量管理规范》(GLP),药物重复给药毒性试验是药物研发体系的有机组成部分,试验设计要重视与其他药理毒理试验设计和研究结果的关联性,要关注同类药物临床使用情况、临床适应症和用药人群、临床用药方案,还要结合受试物理化性质和作用特点,使得重复给药毒性试验结果与其他药理毒理试验研究互为说明、补充或/和印证。 三、基本内容
(一)受试物 中药、天然药物:受试物应采用能充分代表临床试验拟用样品和/或上市样品质量和安全性的样品。应采用工艺路线及关键工艺参数确定后的工艺制备,一般应为中试或中试以上规模的样品,否则应有充分的理由。应注明受试物的名称、来源、批号、含量(或规格)、保存条件、有效期及配制方法等,并提供质量检验报告。由于中药的特殊性,建议现用现配,否则应提供数据支持配制后受试物的质量稳定性及均匀性。当给药时间较长时,应考察配制后体积是否存在随放置时间延长而膨胀造成终浓度不准的因素。如果由于给药容量或给药方法限制,可采用原料药进行试验。试验中所用溶媒和/或辅料应标明名称、标准、批号、有效期、规格及生产单位。 化学药物:受试物应采用工艺相对稳定、纯度和杂质含量能反映临床试验拟用样品和/或上市样品质量和安全性的样品。受试物应注明名称、来源、批号、含量(或规格)、保存条件、有效期及配制方法等,并提供质量检验报告。试验中所用溶媒和/或辅料应标明名称、标准、批号、有效期、规格和生产单位等,并符合试验要求。 在药物研发的过程中,若受试物的工艺发生可能影响其安全性的变化,应进行相应的安全性试验。
急性毒性(GB20592-2006)
化学品分类、警示标签和警示性说明安全规范急性毒性 GB20592-2006 化学品分类、警示标签和警示性说明安全规范急性毒性Safety rules for classification,precautionary labeling and precautionary statements of chemicals-Acute toxicity 前言 本标准第4章、第6章、第7章、第8章为强制性的,其余为推荐性的。 本标准与联合国《化学品分类及标记全球协调制度》(GHS)的一致性程度为非等效,其有关技术内容与GHS中一致,在标准文本格式上按GB/T 1.1—2000做了编辑性修改。 本标准由全国危险化学品管理标准化技术委员会(SAC/TC251)提出并归口。 本标准负责起草单位:天津出入境检验检疫局。 本标准参加起草单位:中国疾病预防控制中心、中化化工标准化研究所、浙江出入境检验检疫局。 本标准主要起草人:王利兵、李宁涛、尚为、冯智颉、刘绍从、张园、陈文。 本标准自2008年1月1日起在生产领域实施;自2008年12
月31日起在流通领域实施,2008年1月1日~12月31日为标准实施过渡期。 化学品分类、警示标签和警示性说明安全规范急性毒性 1 范围 本标准规定了化学品引起的急性毒性的术语和定义、分类、判定流程、类别和警示标签、类别和标签要素的配置及警示性说明的一般规定。 本标准适用于化学品引起的急性毒性按联合国《化学品分类及标记全球协调制度》的危险性分类、警示标签和警示性说明。 2 规范性引用文件 下列文件中的条款通过本标准的引用而成为本标准的条款。凡是注日期的引用文件,其随后所有的修改单(不包括勘误的内容)或修订版均不适用于本标准,然而,鼓励根据本标准达成协议的各方研究是否可使用这些文件的最新版本。凡是不注日期的引用文件,其最新版本适用于本标准。 GB 6944—2005 危险货物分类和品名编号 联合国《化学品分类及标记全球协调制度》(GHS) 联合国《关于危险货物运输的建议书规章范本》 3 术语和定义 急性毒性acute toxicity 经口或经皮肤摄入物质的单次剂量或在24 h内给与的多次剂量,或者4 h的吸入接触发生的急性有害影响。
药物急性毒性试验LD50的方法
精品文档 药物急性毒性试验LD 50的方法 对全新结构的药物或中草药复方,先通过小批量动物的摸索,找出0%和100%估计致 死量(即Dmin和Dmax),再求出i值。 (1)用10倍稀释的药物浓度系列,用少量动物(每组2~3只),找出大致死亡范围。如: 上述结果提示,大致死亡范围为:50~500 mg/kg。 (2)再用1、2、4、8……等2倍稀释的药物浓度系列,每组4只,找出Dmin和Dmax。如: Dmax :当出现4/4死亡时,如其前一组为3/4死亡,则取4/4组的剂量为Dmax ;如前一组为1/4或2/4死亡,考虑到4/4组的剂量在正式实验中可能的死亡率低于70%,为慎重 起见,可将4/4组的剂量乘以2作为Dmax。 Dmax=400 X 70% X 2=560 mg/kg Dmin :当出现0/4死亡时,如其后一组为1/4死亡,则取0/4组的剂量为Dmin ;如后一组大于1/4,考虑到0/4组的剂量在正式实验中可能的死亡率高于70%,为慎重起见,可 将0/4组的剂量除以2作为Dmin。 Dmin=50 十70% 十2~ 35 mg/kg (3)本法用较少的动物和药物,寻找出正式实验时最高死亡率不低于70%,最低死亡率不高于30%点剂量范围在确定了Dmax和Dmin以后,可求得组间距(i值): lg Dmax-lgDmin i= ------------------------------ n-1 (4)以Dmin的对数为起点,向上退出n组动物的各组剂量的对数值,求出反对数即可得出各组的剂量值。 注意:①LD50测定中剂量组数的设计,除符合统计学要求外,还应根据预试验所提供 的药物的毒性情况而定。②一般而言,在实际工作中,设4~5个剂量组,组距以0.65~0.85 为宜。③小鼠每组10只(雌雄各半),大鼠不应少于6~8只。
小鼠的急性毒性试验
五种农药对小鼠的急性毒性试验 绪论 随着现代农业的飞速发展,农药的应用越来越广泛,在农林作物的病虫防治中,农药一直发挥着巨大作用,尤其是本世纪60-70年代,人们大量使用农药,几乎使粮食产量增长一倍,但随着农药长期的、大量的、不合理的使用,导致了对环境的严重污染并对人体健康产生极大的影响。它们对动、植物和人类的危害越来越严重。一方面它们可以直接进入生物体内引起急性、慢性中毒和畸变,同时还通过径流、排污、挥发等途径进入土壤、大气和水体,引起各种生态环境下生物的死亡,并通过食物链的富集影响人类的食品安全。目前,因农药使用与管理失控而引发的一系列水域环境污染以及食品安全等问题,已引起政府相关部门和业内学者的广泛重视。当前,随着有机氯农药的禁用,菊酯类和有机磷类等成为我国目前使用较广泛的农药。 《中华人民共和国农药管理条例》指明,农药是指用于预防、消灭或者控制危害农业、林业的病、虫、草和其他有害生物以及有目的地调节植物、昆虫生长的化学合成物或者几种物质混合物及其制剂。农药残留是指农药使用后残存于环境、生物体和食品中的农药及其衍生物和杂质的总称。动植物在生长期间、食品在加工和流通中均可受到农药的污染,导致食品中农药残留。 相关报道表明,农药利用率一般为10%,约90%的残留在环境中,过多地使用农药,大量未被利用的农药经过降雨、农田渗滤和水田排水等进入水体,同时,还有大量散失的农药挥发到空气中,最后汇入水域,沉降积淀在土壤中,通过农作物吸收和食物链进入人体进行累积,并对人体健康造成危害。目前中国一些食品,如茶叶、大米、肉、蛋等食品中农药残留量常超过规定标准,过多的残留量对人体健康会造成危害。为此,论述农药残留对人体健康的危害效应及其毒理机制和防治措施,以期对防治食品中农药残留对人体健康的危害提供理论依据。 在哺乳类实验动物中,由于小鼠个体小,饲养管理方便,生产繁殖快,质量控制严格,价廉可以大量供应,又有大量的具有各种不同特点的近交品系,突变品系,封闭群及杂交一代动物,小鼠实验研究资料丰富参考对比性强;更重要一点乃是全世界科研工作者均用国际公认的品系和标准的条件进行试验,其实验结果的科学性、可靠性、重复性高,自然会得到国际认可。 本文以百草枯、甲氰菊酯、乐果、草甘膦和敌敌畏五种常用农药为实验材料, 检测了它们对
急性毒性试验
试验目的:急性毒性试验是在24小时内给药1次或2次(间隔6-8小时),观察动物接受过量的受试药物所产生的急性中毒反应,为多次反复给药的毒性试验设计剂量、分析毒性作用的主要靶器官、分析人体过量时可能出现的毒性反应、I期临床的剂量选择和观察指标的设计提供参考信息等。 一、啮齿类动物单次给药的毒性试验 (一)试验条件 1.动物品系:常用健康的小鼠、大鼠。选用其他动物应说明原因。年龄一般为7-9周龄。同批试验中,小鼠或大鼠的初始体重不应超过或低于所用动物平均体重的20%.实验前至少驯养观察1周,记录动物的行为活动、饮食、体重及精神状况。 2.饲养管理:动物饲料应符合动物的营养标准。若用自己配制的饲料,应提供配方及营养成分含量的检测报告;若是购买的饲料,应注明生产单位。应写明动物饲养室内环境因素的控制情况。 3.受试药物:应注明受试药物的名称、批号、来源、纯度、保存条件及配制方法。 (二)试验方法: 由于受试药物的化学结构、活性成分的含量、药理、毒理学特点各异,毒性也不同,有的很难观察到毒性反应,实验者可根据受试药物的特点,由下列几种实验方法中选择一种进行急性毒性试验。 1.伴随测定半数致死量(LD50)的急性毒性试验方法。 2.最大耐受剂量(MTD)试验方法:最大耐受剂量,是引起动物出现明显的中毒反应而不产生死亡的剂量。 3.最大受试药物量试验方法:在合理的浓度及合理的容量条件下,用最大的剂量给予实验动物,观察动物的反应。 4.单次口服固定剂量方法(Fixed-dose procedure)。选择5、50、500和2000mg/kg四个固定剂量。 实验动物首选大鼠,给药前禁食6-12小时,给受试药物后再禁食3-4小时。如无资料证明雄性动物对受药试物更敏感,首先用雌性动物进行预试。根据受试药物的有关资料,由上述四个剂量中选择一个作初始剂量,若无有关资料作参考,可用500mg/kg作初始剂量进行预试,如无毒性反应,则用2000mg/kg 进行预试,此剂量如无死亡发生即可结束预试。如初始剂量出现严重的毒性反应,那就用下一个挡次的剂量进行预试,如该动物存活,就在此两个固定剂量之间选择一个中间剂量试验。每个剂量给一只动物,预试一般不超过5只动物。每个剂量试验之间至少应间隔24小时。给受试药物后的观察期至少7天,如动物的毒性反应到第7天仍然存在,尚应继续再观察7天。 在上述预试的基础上进行正式试验。每个剂量最少用10只动物,雌雄各半。根据预试的结果,由前面所述的四种剂量中选择出可能产生明显毒性但又不引起死亡的剂量;如预试结果表明,50mg/kg引起死亡,则降低一个剂量档次试验。
实验二 经口急性毒性试验
毒理学实验二经口急性毒性试验 一、实验目得 1、掌握实验动物分组方法 2、测定LD50得试验设计原则 3、小鼠得经口灌胃技术 二、试剂与材料 1、实验动物: (1)动物品种:健康成年ICR小鼠,体重18g~22g (2)样品来源:首都医科大学实验动物部 2、器材:注射器(1ml)、灌胃针头、烧杯、吸管、容量瓶、烧杯、棉签、动物秤。 3、试剂:敌敌畏(1400mg/ml)、苦味酸染液(标记用)。 三、实验内容 1、健康实验动物得选择与性别鉴定 选择健康得雄性小鼠(健康标准:毛顺、毛顺、无分泌物、反应敏锐。动物出现圆圈动作可能为中耳炎,废弃。) 肛门与生殖孔距离:大者为雄性,小者为雌性 2、实验动物称重、编号与随机分组 选择体重在18-22 g得小鼠,采用随机分组得方法(动物按体重分为几个体重段,再从每个体重段分出各组动物),每组10只小鼠,用黄色得苦味酸饱与液标号1 ~9,10号小鼠不标记、 3、受试化学物溶液得配制 (1)确定灌胃量:0、1ml/10g (2)确定最高给药量,计算溶液浓度,估计给药总体积 (3)药品称量及稀释 4、小鼠灌胃技术 左手固定,右手持灌胃器,插入动物口腔,沿咽后壁徐徐插入食道,深度为口腔至剑突得距离。 5、毒性体征得观察与LD50计算 (1)毒性体征得观察: 染毒后注意观察小鼠中毒得发生、发展过程及死亡数与死亡时间 按表格记录动物体征及出现时间,记录死亡情况及时间,观察期为30 min (2)LD50得计算: a、实验各组剂量得确定:设5组,每组雌雄动物各10只。 剂量组距 d 为: d为相邻两个剂量组剂量对数之差 利用lgLD0依次加d,取反对数,即可得出各组剂量。 b、LD50得计算(见附件):
鱼的急性毒性试验
鱼的急性毒性试验 一、实验目的和要求: 通过本试验,熟悉和掌握鱼类急性毒性试验的设计、条件、操作步骤,以及试验结果的计算、分析和报告等全过程。 二、实验原理: 鱼类对水环境的变化反应十分灵敏,当水体中的污染物达到一定程度时,就会引起一系列中毒反应,例如行为异常、生理功能紊乱、组织细胞病变直至死亡。在规定的条件下,使鱼接触含不同浓度受试物的水溶液,实验至少进行24h,最好以96h为一个实验周期,在24h、48h、72h、96h时记录实验鱼的死亡率,确定鱼类死亡50%时的受试物浓度。鱼类毒性试验在研究水污染及水环境质量中占重要地位。通过鱼类急性毒性试验可以评价受试物仅用于测定化学物质毒性强度、测定水体污染程度、检查废水处理的有效成都,也为制定水质标准、评价环境质量和管理废水排放提供环境依据。 三、实验材料: 1.实验鱼的选择和驯养 12×6 小锦鲤鱼体长7-12cm 体宽3-5cm 体重 7-12g 不同浓度的苯酚(mg/L)0、24、48、96、192、384 2、实验仪器设备 (1)实验容器 实验容器一般用玻璃或其他化学惰性材质制成的水槽。容器体积可以根据试验鱼的体重确定,通常以每升水中鱼的负荷不得超过2g(最好为1g)。一些小型鱼类幼鱼可选择500ml 或1000ml烧杯为实验容器。容器的深度必须超过16cm,水体表面积越大越好。同一实验应采用相同规格和质量的容器。为防止鱼类跳出容器,可在容器上加上网罩。实验容器使用后,必须彻底洗净,以除去所有毒性残留物。 (2)其他 吸光光度计 3、实验用水:曝气水 四、操作步骤: 1、设置5个浓度组,1个空白对照组,选择不同浓度的苯酚(mg/L)0、24、48、96、 192、384。每个浓度放入12条小锦鲤鱼。采用直接投毒方式,将配制的苯酚溶液直接倒入水槽中,搅拌均匀。分别分为1、2、3、4、5、6组。染毒后观察其活动状况,并
实验二-经口急性毒性试验
毒理学实验二经口急性毒性试验 一、实验目的 1、掌握实验动物分组方法 2、测定LD50的试验设计原则 3、小鼠的经口灌胃技术 二、试剂和材料 1、实验动物: (1)动物品种:健康成年ICR小鼠,体重18g~22g (2)样品来源:首都医科大学实验动物部 2、器材:注射器(1ml)、灌胃针头、烧杯、吸管、容量瓶、烧杯、棉签、动物秤。 3、试剂:敌敌畏(1400mg/ml)、苦味酸染液(标记用)。 三、实验内容 1、健康实验动物的选择和性别鉴定 选择健康的雄性小鼠(健康标准:毛顺、毛顺、无分泌物、反应敏锐。动物出现圆圈动作可能为中耳炎,废弃。) 肛门与生殖孔距离:大者为雄性,小者为雌性 2、实验动物称重、编号和随机分组 选择体重在18-22 g的小鼠,采用随机分组的方法(动物按体重分为几个体重段,再从每个体重段分出各组动物),每组10只小鼠,用黄色的苦味酸饱和液标号1~9,10号小鼠不标记。 3、受试化学物溶液的配制 (1)确定灌胃量:0.1ml/10g (2)确定最高给药量,计算溶液浓度,估计给药总体积 (3)药品称量及稀释 4、小鼠灌胃技术 左手固定,右手持灌胃器,插入动物口腔,沿咽后壁徐徐插入食道,深度为口腔至剑突的距离。 5、毒性体征的观察和LD50计算 (1)毒性体征的观察: 染毒后注意观察小鼠中毒的发生、发展过程及死亡数和死亡时间 按表格记录动物体征及出现时间,记录死亡情况及时间,观察期为30 min
组数 :各组死亡率:数相邻两组对数剂量之差:最大剂量的对数 P d :X )P P (d 21X lg 150i i k i i k LD ∑++-=)lg 96.1(lg lg 95%:1)P 1(P d lg 50501-50LD S LD ni ni LD S i i ±--=∑可信区间:实验动物数。标准误公式: (2)LD50的计算: a 、实验各组剂量的确定:设5组,每组雌雄动物各10只。 剂量组距 d 为: d 为相邻两个剂量组剂量对数之差 利用lgLD0依次加d ,取反对数,即可得出各组剂量。 b 、LD50的计算(见附件): C 、求半数致死量的95%可信区间 四、实验过程 1、人员分工:本次实习同学分两个大组(A 组和B 组),分别在不同实验室。每大组分5个小组,分别处理雌雄动物,每小组10只动物。 集体活动:1、 2、 3、 4、5 组各1人,进行受试物配制。 1 lg lg d 0100--=组数LD LD
实验二 经口急性毒性试验
毒理学实验二经口急性毒性试验 1、实验目的 1、掌握实验动物分组方法 2、测定LD50的试验设计原则 3、小鼠的经口灌胃技术 二、试剂和材料 1、实验动物: (1)动物品种:健康成年ICR小鼠,体重18g~22g (2)样品来源:首都医科大学实验动物部 2、器材:注射器(1ml)、灌胃针头、烧杯、吸管、容量瓶、烧杯、棉签、动物秤。 3、试剂:敌敌畏(1400mg/ml)、苦味酸染液(标记用)。 3、实验内容 1、健康实验动物的选择和性别鉴定 选择健康的雄性小鼠(健康标准:毛顺、毛顺、无分泌物、反应敏锐。动物出现圆圈动作可能为中耳炎,废弃。) 肛门与生殖孔距离:大者为雄性,小者为雌性 2、实验动物称重、编号和随机分组 选择体重在18-22 g的小鼠,采用随机分组的方法(动物按体重分为几个体重段,再从每个体重段分出各组动物),每组10只小鼠,用黄色的苦味酸饱和液标号1~9,10号小鼠不标记。 3、受试化学物溶液的配制 (1)确定灌胃量:0.1ml/10g (2)确定最高给药量,计算溶液浓度,估计给药总体积 (3)药品称量及稀释 4、小鼠灌胃技术 左手固定,右手持灌胃器,插入动物口腔,沿咽后壁徐徐插入食道,深度为口腔至剑突的距离。 5、毒性体征的观察和LD50计算 (1)毒性体征的观察:
染毒后注意观察小鼠中毒的发生、发展过程及死亡数和死亡时间 按表格记录动物体征及出现时间,记录死亡情况及时间,观察期为30 min (2) LD50的计算: a、实验各组剂量的确定:设5组,每组雌雄动物各10只。 剂量组距 d 为: d为相邻两个剂量组剂量对数之差 利用lgLD0依次加d,取反对数,即可得出各组剂量。 b、LD50的计算(见附件): C、求半数致死量的95%可信区间 4、实验过程 1、人员分工:本次实习同学分两个大组(A组和B组),分别在不同实验室。每大组分5个小组,分别处理雌雄动物,每小组10只动物。 集体活动:1、 2、 3、 4、5 组各1人,进行受试物配制。 各小组活动: 每小组1人(共4人),进行动物标记。(1-10号) 每小组1人(共4人),进行体重记录。(1-10号) 每小组1人(共4人),进行灌胃。(1-10号) 每小组1人(共4人),根据体重吸取受试物(0.1ml/10g)
急性毒性试验[1]
实验一急性毒性试验(Acute Cytotoxicity Test) 一、实验目的: 了解生物材料急性毒性的含义,掌握急性毒性试验的基本方法。 二、实验原理: 医学上通常指的急性毒性试验是对药物而言的,并以半数致死量(median lethal dose, LD50)来衡量药物急性毒性的大小。所谓LD50是指某一药物使试验动物总体死亡一半的剂量,由于LD50是剂量反应曲线上最敏感的一点,而且有易测、准确和重复性好的优点,以此作为药物使用的安全指标。但对于生物材料而言,它与药物在体内的反应机理不同,大多数生物材料不能计算LD50,所以在试验过程中,通过对实验动物进行动物静脉或腹腔注射试验材料或其浸提液来观察实验动物体重在24、48和72h的变化、运动、呼吸状态以及死亡情况作为评价的指标,判定某种生物材料的急性毒性作用。 三、实验对象:小鼠 四、实验器材和药品: 聚甲基丙烯酸羟乙酯(PHEMA),蒸馏水,生理盐水(0.9%),注射器(1ml),量筒(10ml),小烧杯(50、100ml),高压消毒器。 五、实验步骤: 1.浸提液制备: 按评价标准裁剪试样,选择适当浸提温度制备浸提液。 2.将10只体重在17~23g间的健康、未做过其他实验的小鼠随机分为实验组和对照组,每组5只。 3.将浸提液按每公斤小鼠体重注射50ml于实验组小鼠尾静脉(50ml/kg),用生理盐水按同样方法作空白对照。 4.记录试样表面积和使用浸提液的容量;记录注射后24h、48h、72h两组小鼠的体重,观察其各种生物学反应情况。 六、评价方法:
2.结果判断标准: 2.1 在72h观察期内,注射材料浸提液的动物反应不大于对照组动物,则认为该材料符合急性毒性试验要求。 2.2在72h观察期内,注射材料浸提液动物中有2只以上出现轻度毒性症状或仅1只动物出现明显毒性症状死亡,或实验组5只动物的体重均下降,即使无其他中毒症状都要进行重复试验。 2.3 重复试验的动物数量应加倍,即每组需10只小鼠。浸提液应该重新制备。重复试验若符合2.1 项要求,则认为该材料合格。 2.4 如实验组动物有2只以上发生死亡或3只以上出现明显毒性症状或动物普遍出现进行性体重下降,则不需要重复试验,可认为该材料不符合急性毒性试验要求。 附:小鼠静脉注射方法 小鼠的尾部有三条静脉,一般采用两侧的静脉。把动物固定在暴露尾部的固定器内(可用烧杯、铁丝罩或粗试管邓物代替固定器)。拔去尾部静脉走向的毛,置尾巴于40~500C 温水中浸泡几分钟,或用75%乙醇棉球反复擦抹,使尾部血管扩张。行尾部注射时,尽量采用与尾部平行的角度进针,抽吸法不能验证是否穿刺成功,开始注药时应尽量缓慢,仔细观察,如果有白色皮丘出现,说明未刺入血管,应重新向尾部方向移动针头,再次穿刺,直至注射时无皮丘出现,才能正式注射药物,有时在注射药物的同时可见静脉血被进去的药物向前推进。 实验二致热源试验(hypersusceptibility test) 一、实验目的: 掌握致热源实验的基本方法。 二、实验原理: 致热源试验是通过被测材料或其浸提液注入实验动物体内,若浸提液存在热源物质,作用于单核细胞、巨噬细胞等靶细胞后,促使其产生内出性热源,作用于丘脑体温调节中枢,使动物体温上升,因此,观察动物的体温变化可用来判断该材料或其浸提液中所含热源量是否符合人体的要求。 三、实验对象:兔 四、实验器材和药品: 硅橡胶、蒸馏水、生理盐水(0.9℅)、注射器(50ml)、烧杯(150ml)、量筒(100ml)、高压消毒器、体温计(肛测)。 五、实验步骤: 1.浸提液制备: 1.1将所有与浸提液接触的容器、量器等玻璃器皿均应先置于干燥箱内250℃加热30min,或180℃加热2h去除热原物质。 1.2 浸提液所用灭菌0.9℅生理盐水应是热原检查合格者,试样浸提前应用同一批号灭
急性毒性试验
急性毒性试验 试验目的:急性毒性试验是在24小时内给药1次或2次(间隔6-8小时),观察动物接受过量的受试药物所产生的急性中毒反应,为多次反复给药的毒性试验设计剂量、分析毒性作用的主要靶器官、分析人体过量时可能出现的毒性反应、I期临床的剂量选择和观察指标的设计 提供参考信息等。 一、啮齿类动物单次给药的毒性试验 (一)试验条件 1.动物品系:常用健康的小鼠、大鼠。选用其他动物应说明原因。年龄一般为7-9周龄。同批试验中,小鼠或大鼠的初始体重不应超过或低于所用动物平均体重的20%。实验前至少驯养观察1周,记录动物的行为活动、饮食、体重及精神状况。 2.饲养管理:动物饲料应符合动物的营养标准。若用自己配制的饲料,应提供配方及营养成分含量的检测报告;若是购买的饲料,应注明生产单位。应写明动物饲养室内环境因素的控 制情况。 3.受试药物:应注明受试药物的名称、批号、来源、纯度、保存条件及配制方法。 (二)试验方法: 由于受试药物的化学结构、活性成分的含量、药理、毒理学特点各异,毒性也不同,有的很难观察到毒性反应,实验者可根据受试药物的特点,由下列几种实验方法中选择一种进行急 性毒性试验。 1.伴随测定半数致死量(LD50)的急性毒性试验方法。 2.最大耐受剂量(MTD)试验方法:最大耐受剂量,是引起动物出现明显的中毒反应而不产
生死亡的剂量。 3.最大受试药物量试验方法:在合理的浓度及合理的容量条件下,用最大的剂量给予实验动 物,观察动物的反应。 4.单次口服固定剂量方法(Fixed-dose procedure)。选择5、50、500和2000mg/kg四个 固定剂量。 实验动物首选大鼠,给药前禁食6-12小时,给受试药物后再禁食3-4小时。如无资料证明雄性动物对受药试物更敏感,首先用雌性动物进行预试。根据受试药物的有关资料,由上述四个剂量中选择一个作初始剂量,若无有关资料作参考,可用500mg/kg作初始剂量进行预试,如无毒性反应,则用2000mg/kg进行预试,此剂量如无死亡发生即可结束预试。如初始剂量出现严重的毒性反应,那就用下一个挡次的剂量进行预试,如该动物存活,就在此两个固定剂量之间选择一个中间剂量试验。每个剂量给一只动物,预试一般不超过5只动物。每个剂量试验之间至少应间隔24小时。给受试药物后的观察期至少7天,如动物的毒性反应到第7 天仍然存在,尚应继续再观察7天。 在上述预试的基础上进行正式试验。每个剂量最少用10只动物,雌雄各半。根据预试的结果,由前面所述的四种剂量中选择出可能产生明显毒性但又不引起死亡的剂量;如预试结果表明,50mg/kg引起死亡,则降低一个剂量档次试验。 试验观察:给受试药物后至少应观察2周,根据毒性反应的具体特点可适当延长。对每只动物均应仔细观察和详细记录各种毒性反应出现和消失的时间。给受试药物当天至少应观察记录两次,以后可每天一次。观察记录的内容包括皮肤、粘膜、毛色、眼睛、呼吸、循环、自主及中枢神经系统行为表现等。动物死亡时间的记录要准确。给受试药物前、给受试药物后1周、动物死亡及试验结束时应称取动物的体重。所有动物包括死亡或处死的动物均应进行尸检,尸检异常的器官应作病理组织学检查。固定剂量试验法所获得的结果,参考下表标准进 行评价。 单次口服固定剂量试验法结果的评价
药物毒性试验的设计
Optimising the design of preliminary toxicity studies for pharmaceutical safety testing in the dog David Smith a, , , Robert Combes b, Olympe Depelchin c, Soren Dyring Jacobsen d, Ruediger Hack e, Joerg Luft f, Lieve Lammens g, Friedrich von Landenberg h, Barry Phillips i, Rudolf Pfister j, Yvon Rabemampianina k, Susan Sparrow l, Claudia Stark m and Markus Stephan-Gueldner n a AstraZeneca, Alderley Park, UK b FRAME, Nottingham, UK c Lilly, Mont-Saint Guibert, Belguim d NovoNordisk, Maaloev, Denmark e Aventis, Frankfurt, Germany f AltanaPharma, Hamburg, Germany g Janssen, Beerse, Belgium h Merck KGaA, Darmstadt, Germany i RSPCA, Horsham, UK j Novartis Pharma, Basel, Switzerland k Pfizer, Amboise, France l GlaxoSmithKline, Ware, UK m Schering AG, Berlin, Germany n Hoffmann-La Roche AG, Basel, Switzerland Abstract A working party, comprising two animal welfare organisations and some 12 pharmaceutical companies in Europe, was established to minimise the use of the dog in safety testing. As first step, the participants defined the major objectives of preliminary dose-range finding/MTD toxicity studies in non-rodents, defined the principles and requirements for this study type and agreed on a proposal for an optimised study design, based on collective experience of conducting such studies in industry, involving an evaluation of 100 individual study data sets. The suggested study design is explained and described, and reflects current best practice in the pharmaceutical industry in Europe. The implementation of such an optimised design is believed to result in a reduction in the overall numbers of animals used for this purpose, without jeopardising the scientific rationale and
急性毒性试验方法
由于受试药物的化学结构、活性成分的含量、药理、毒理学特点各异,毒性也不同,有的很难观察到毒性反应,实验者可根据受试药物的特点,由下列几种实验方法中选择一种进行急性毒性试验。 1.伴随测定半数致死量(LD50)的急性毒性试验方法。 2.最大耐受剂量(MTD)试验方法:最大耐受剂量,是引起动物出现明显的中毒反应而不产生死亡的剂量。3.最大受试药物量试验方法:在合理的浓度及合理的容量条件下,用最大的剂量给予实验动物,观察动物的反应。 4.单次口服固定剂量方法(Fixed-dose procedure)。选择5、50、500和2000mg/kg四个固定剂量。 实验动物首选大鼠,给药前禁食6-12小时,给受试药物后再禁食3-4小时。如无资料证明雄性动物对受药试物更敏感,首先用雌性动物进行预试。根据受试药物的有关资料,由上述四个剂量中选择一个作初始剂量,若无有关资料作参考,可用500mg/kg作初始剂量进行预试,如无毒性反应,则用2000mg/kg进行预试,此剂量如无死亡发生即可结束预试。如初始剂量出现严重的毒性反应,那就用下一个挡次的剂量进行预试,如该动物存活,就在此两个固定剂量之间选择一个中间剂量试验。每个剂量给一只动物,预试一般不超过5只动物。每个剂量试验之间至少应间隔24小时。给受试药物后的观察期至少7天,如动物的毒性反应到第7天仍然存在,尚应继续再观察7天。 在上述预试的基础上进行正式试验。每个剂量最少用10只动物,雌雄各半。根据预试的结果,由前面所述的四种剂量中选择出可能产生明显毒性但又不引起死亡的剂量;如预试结果表明,50mg/kg引起死亡,则降低一个剂量档次试验。
药物毒性试验的设计
Optimising the design of preliminary toxicity studies for pharmaceutical safety testing in the dog David Smith a, , , Robert Combes b , Olympe Depelchin c , Soren Dyring Jacobsen d , Ruediger Hack e , Joerg Luft f , Lieve Lammens g , Friedrich von Landenberg h , Barry Phillips i , Rudolf Pfister j , Yvon Rabemampianina k , Susan Sparrow l , Claudia Stark m and Markus Stephan-Gueldner n a AstraZeneca, Alderley Park, UK b FRAME, Nottingham, UK c Lilly, Mont-Saint Guibert, Belguim d NovoNordisk, Maaloev, Denmark e Aventis, Frankfurt, Germany f AltanaPharma, Hamburg, Germany g Janssen, Beerse, Belgium h Merck KGaA, Darmstadt, Germany i RSPCA, Horsham, UK j Novartis Pharma, Basel, Switzerland k Pfizer, Amboise, France l GlaxoSmithKline, Ware, UK m Schering AG, Berlin, Germany n Hoffmann-La Roche AG, Basel, Switzerland Abstract A working party, comprising two animal welfare organisations and some 12 pharmaceutical companies in Europe, was established to minimise the use of the dog in safety testing. As first step, the participants defined the major objectives of preliminary dose-range finding/MTD toxicity studies in non-rodents, defined the principles and requirements for this study type and agreed on a proposal for an optimised study design, based on collective experience of conducting such studies in industry, involving an evaluation of 100 individual study data sets. The suggested study design is explained and described, and reflects current best practice in the pharmaceutical industry in Europe. The implementation of such an optimised design is believed to result in a reduction in the overall numbers of animals used for this purpose, without jeopardising the scientific rationale and b b s .y a o z h .c o m
药物急性毒性实验
实验一药物急性半数致死量(LD50)的测定 【目的】 了解药物半数致死量(LD50)测定的意义、原理,掌握半数致死量的测定方法和计算过程。【原理】 LD50是指在一群动物中能使半数动物死亡的剂量。由于实验动物的抽样误差,药物的致死量对数值大多在50%质反应的上下呈正态分布。在这样的质反应中药物剂量和质反应间呈S型曲线,S型曲线的两端处较平,而在50%质反应处曲线斜率最大,因此这里的药物剂量稍有变动,则动物的死或活的反应出现明显差异,所以测定半数致死量能比较准确地反映药物毒性的大小。 【实验材料】 1、动物:小白鼠,体重18-24g,雌、雄各半,实验前禁食12小时,不禁水。 2、药品:盐酸普鲁卡因,苦味酸。 3、器械:小鼠笼,天平,注射器(1mL),电子计算器。 【方法和步骤】 (一)预备实验 1、探索剂量范围:先找出100%及0%死亡的剂量,此即上下限剂量(D m及D n)。方法是先取出小鼠9-12只,每组3只,按估计量(根据经验或文献资料定出)给药,如3只小鼠全死则降低剂量一半,如全不死则增加剂量一倍,如部分死亡,则按2:1的比例向上、向下调整剂量,由此找出上下限剂量。 2、确定组数,计算各组剂量: 确定组数(G):可根据适宜的组距确定组数,一般分5-8个剂量组。 计算各组剂量:要求各组剂量按等比级数排列,在找出D m及D n和确定组数后,可按下列公式求出公比r: r 再按公比计算各组剂量D1,D2,D3,D4,D5……D m,其中D1=D n=最小剂量,D2=D1?r; D3=D2?r; D4=D3?r; D5=D4?r; ……D G=D G-1?r。r值一般以1.7~1.15之间为宜。 计算举例:已知某药在致死毒性实验中,Dm=187.5 mg/kg; Dn=76.8 mg/kg, 确定组数 G=5,求r及各组剂量。先代入公式求r=1.25,再计算各组剂量D1=Dn=76.8 mg/kg, D2=76.8?1.25=96 mg/kg, 依次计算D3,D4,及D G(D5)分别为120,150,187.5 mg/kg。
中药急性毒性实验简介
中药急性毒性实验简介 动物急性毒性实验研究目的:阐明药物的毒性作用;了解其毒性靶器官;长期毒性实验剂量参考;药效学研究的剂量的设计依据;临床实验起始剂量的参考 受试物: 用于申报新药的受试物应采用制备工艺稳定,符合临床试验用质量标准规定的中试样品。 如果由于给药容量或给药方法限制,可以采用原料药进行试验。 实验动物: 通常采用哺乳动物进行实验; 通常选用雌雄各半(临床为单性别用药除外); 年龄和体重:一般采用健康成年动物(如临床拟用于儿童,采用幼年动物); 初始体重不应偏离平均体重的20%。 给药途径: 可采用不同给药途径,但其中包括与拟临床给药途径一致的给药途径。 经口给药时必须禁食不禁水过夜。 给药容量: 小鼠一次不超过40ml/kg,大鼠一次给药容量不超过20ml/kg。 观察期限 一般为14天,如果毒性反应较慢应延长观察时间。 观察指标 动物体重变化,饮食,外观,行为,分泌物,排泄物,死亡情况,中毒反应等。 对死亡动物应及时进行大体解剖,器官异常时进行组织病理学检查。 结果处理和分析 根据所观察到的各种反应出现的时间、严重程度、持续时间等,分析各种反应在不同剂量时的反应率、反应程度。 判断出可能涉及的组织、器官和系统以及毒性靶器官等。 根据急性毒性实验结果,结合其他安全性实验、有效性实验等,分析其开发前景。 通常测定的毒性剂量 最大给药量,最大无毒剂量,最大耐受量,致死量(LD50,LD5)等。 通常测定的毒性反应剂量: 最大给药量: 单次或24h内2-3次(间隔4-6h一次)给予的最大给药剂量(合理的最大给药浓度,最大给药容量),观察动物出现的反应。 中药及复方制剂急性毒性研究中常用。
急性毒性实验参考
小鼠口服枸橼酸托烷司琼原料急性毒性试验 摘要 小鼠一次灌胃枸橼酸托烷司琼原料,连续观察14天。观察行为反应并记录死亡情况。死亡小鼠解剖可见心脏瘀血。存活者第15天全部解剖,肉眼检查主要脏器未见明显病变。其死亡率用Bliss法求得枸橼酸托烷司琼LD50 为418.29 mg/kg;95%可信限为390.74 ~447.79 mg/kg。 1.0 实验目的 观察受试物一次口服对小鼠产生的急性毒性反应和死亡情况。 2.0 受试物 2.1 名称:枸橼酸托烷司琼原料,白色粉末。 2.2 提供单位:中国科学院上海药物研究所朱友成组 2.3 批号: 9902 2.4 含量:99.7% 2.5 配制方法:将受试药物用0.5%CMC-Na 研磨配制成混悬液,并稀释成相应浓度,使各剂量组给药体积相等。 2.6 溶剂:0.5%CMC-Na 3.0 动物 3.1 来源、种属、合格证:昆明种小鼠60只,(♀30只,♂30只)由中国科学院上海实验动物中心提供,合格证:中科动管第005号。 经一周适应性饲养。饲料购自中英合资上海西普尔-必凯实验动物有限公司。自由取水,饲养温度为23±2℃。 3.2 体重:给药时体重为18-22克。 3.3 性别:雌雄各半。
3.4 每组动物数:按体重随机分组,实验时以每10只(♀5只,♂5只)为一组。 4.0 剂量 4.1 剂量设置:按预初实验结果,最高剂量定为570 mg/kg。以0.9的比例递减,即为570、513、461.7、41 5.5、374、33 6.6 mg/kg,6个剂量组。 4.2 每只动物接受容量:口服体积为0.2 ml/10g 体重。 5.0 给药途径 小鼠禁食6 小时一次灌胃给药。 6.0 方法 动物按体重随机分6组,每组10只,雌雄各半,每组的小鼠体重分布相似。给药后即观察动物各方面反应情况,死亡动物即进行解剖,检查内脏。记录每天动物的死亡数。 7.0 观察指标 7.1 观察期:14天 7.2 毒性反应:观察检查小鼠外观、行为、进食、粪便等情况,死亡动物进行尸解。第15天实验结束时,存活小鼠解剖,检查心、肺、肝、脾、肾等脏器病变。 8.0 结果 8.1 毒性反应及死亡原因:小鼠灌胃枸橼酸托烷司琼原料后,高剂量组(570、513 mg/kg) 药后5分钟左右安静,活动减少、趴地,15分钟左右全身抖动、抽搐死亡。大部分死亡发生在24 h内。死亡小鼠解剖肉眼检查发现心脏瘀血。存活小鼠第15天解剖,肉眼检查各脏器未见明显病变。
